“We are basically doing what a public health agency should be doing.”
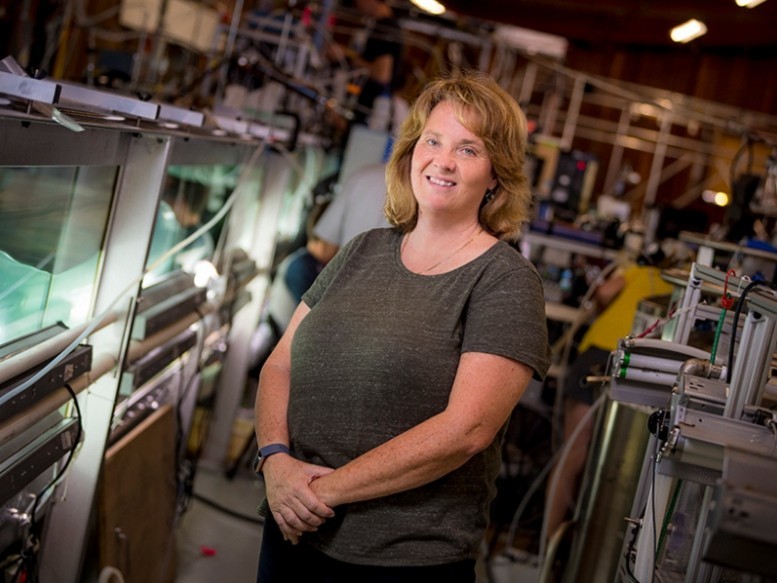
Kim Prather stands next to a wave tank in San Diego, Calif. She pivoted from pollution to COVID-19 research last year. “It’s so frustrating because we’re all scrambling.…We cannot keep doing this.” Credit: UC San Diego Publications/Erik Jepsen
Atmospheric chemist Kimberly Prather wants her day job back.
As a professor at Scripps Institution of Oceanography, she usually spends her days looking at pollution in the ocean and its effects on human health. But since the outbreak of the coronavirus, Prather has dedicated herself to understanding the airborne spread of the virus.
Since the airborne droplets that spread coronavirus are chemically similar to sea spray, Prather was well poised to pivot her work. “We’re very interested in viruses and bacteria that start out in the ocean, but when waves crash, they get enriched into the atmosphere,” explained Prather.
“I’ve been contacted by people in the health care industry, including dental assistants,” she said. “They’re desperate.”
In response, Prather and others created an open-source document of frequently asked questions (FAQ) about airborne spread. They’ve written letters to officials and called out medical science that they say is at odds with physics. They’ve also repurposed their labs or work spaces for COVID-19 research, like one scientist in Colorado who repurposed instruments from his team’s airplane and coughed on them in the lab.
“I’ve gotten a ridiculous number of thank-you letters from all over the world saying how many lives I’ve saved,” Prather said. “That’s nice, but…I want this thing to end.”
Help to the Public, Appeals to Agencies
“We think that unfortunately, [the World Health Organization (WHO)] and CDC are being too slow to accept aerosol transmission, hence the need for these FAQs directly from the scientists” begins the 62-page document written by Prather and 11 other scientists. The FAQ sheet answers questions on ride-sharing, elevators, masks, and air filtration, among other topics.
The WHO and Centers for Disease Control and Prevention (CDC) did not respond to requests for comment on this article.
Last month, Prather and 11 colleagues sent a letter warning the Biden administration that workers in health care, food processing, security, and prison populations aren’t adequately protected from the virus.
They claim that although the CDC has acknowledged that people could contract COVID-19 through inhaling particles, they haven’t updated their guidance. For example, the agency recommends that health care workers wear surgical masks, even when the United States has more effective N95 masks available.
At Odds with Basic Science
Medical textbooks have descriptions of virus transmission that are not consistent with basic physics, said Jose-Luis Jimenez, an atmospheric chemist at the University of Colorado Boulder.
The WHO says that big droplets of human exhalations are the primary mode of transmission for the virus. The agency calls them respiratory droplets and defines them as anything larger than 5 micrometers, about the size of a red blood cell.
But WHO’s definition of respiratory droplets is wrong, said Jimenez. Cloud droplets are around 20 micrometers and they don’t fall to the ground, he said. That means that droplets of larger size could be airborne longer than the WHO acknowledges.
“It’s just absurd,” said Jimenez. “This still is the official statement of the WHO, and they have refused to correct it for a year.”
The break in identifying transmission droplets should be 100 micrometers, argued Prather in a letter in Science last year. The argument isn’t just semantics: It directly affects safety measures.
But CDC and WHO guidelines emphasize that most transmission is passed through close contact, not airborne transmission. “The balance of attention must be shifted to protecting against airborne transmission,” Prather wrote.
Concerned for Family
At the start of the pandemic, atmospheric scientist Jorgen Jensen repurposed a sensor from an aircraft that his team uses to measure cloud particles. He wanted to know how humidity in the air affected aerosols, so he exhaled and coughed onto microscope slides in his lab at the National Center for Atmospheric Research in Boulder, Colo. He then tweaked the humidity in the air surrounding the slides.
He found that humidity affects the size of the droplet over time. Droplets from human exhalations are salty, and drying them out makes the droplet increasingly uninhabitable to viruses. But if a droplet dries out completely, the virus can remain viable for much longer.
While doing his research, Jensen thinks of his father, living in a poorly ventilated nursing home in Denmark. He wants to know what humidity range nursing homes could use to minimize person-to-person transmission. He said that his preliminary research shows that there is a Goldilocks spot of air—not too humid and not too dry—that could thwart airborne viruses faster.
Jensen partnered with aerobiology engineer Mark Hernandez at the University of Colorado Boulder to test the viability of virus particles.
“We were all baffled that [public health agencies] didn’t take aerosol transmission as being more serious to begin with,” said Jenson.
“There were people who were hammering that, and they were not being heard for many, many months,” said Jenson. “And my personal feeling is that was a tragedy.”
—Jenessa Duncombe (@jrdscience), Staff Writer


